The TULSA Procedure unfolds in four basic stages:
Before anything else, the patient sits down with the treatment team, which usually includes a urologist and/or a radiologist, an anesthesiologist, and a few radiology techs. They’ll run through the steps one more time, answer any last questions, and make sure the patient is relaxed before giving sedation.
Once the patient is comfortable, the team wheels the treatment table into the MRI room. Here, the ultrasound applicator (UA) is gently slid into the urethra, and the endorectal cooling device (ECD) is placed into the rectum.
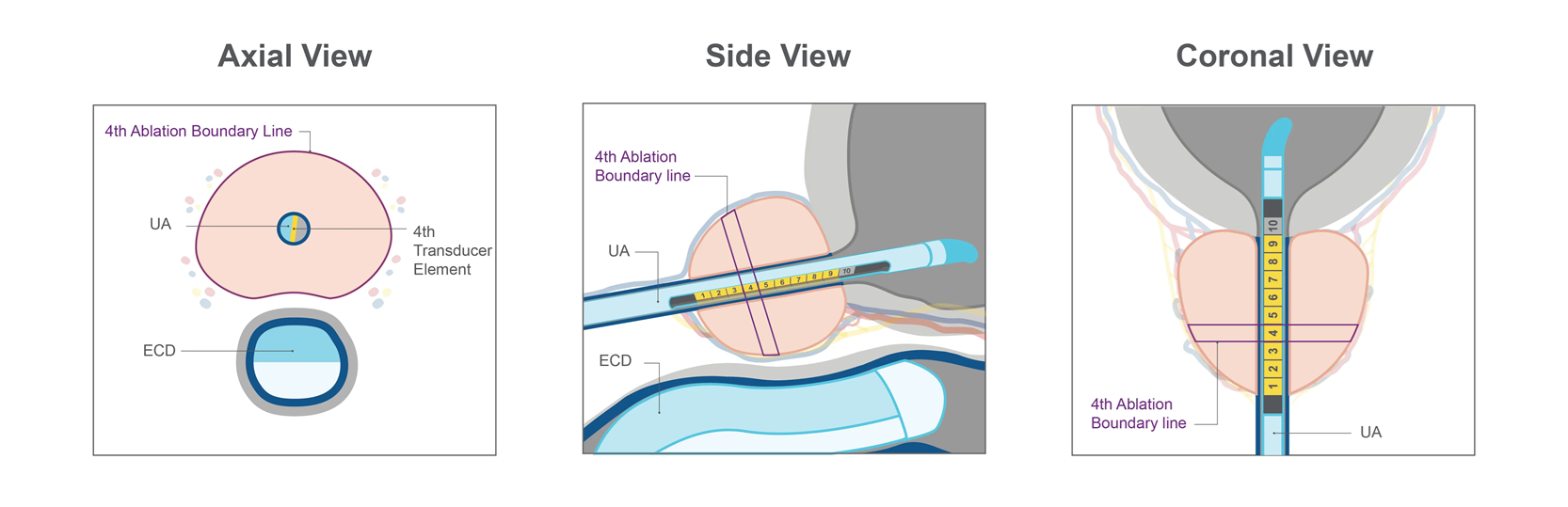
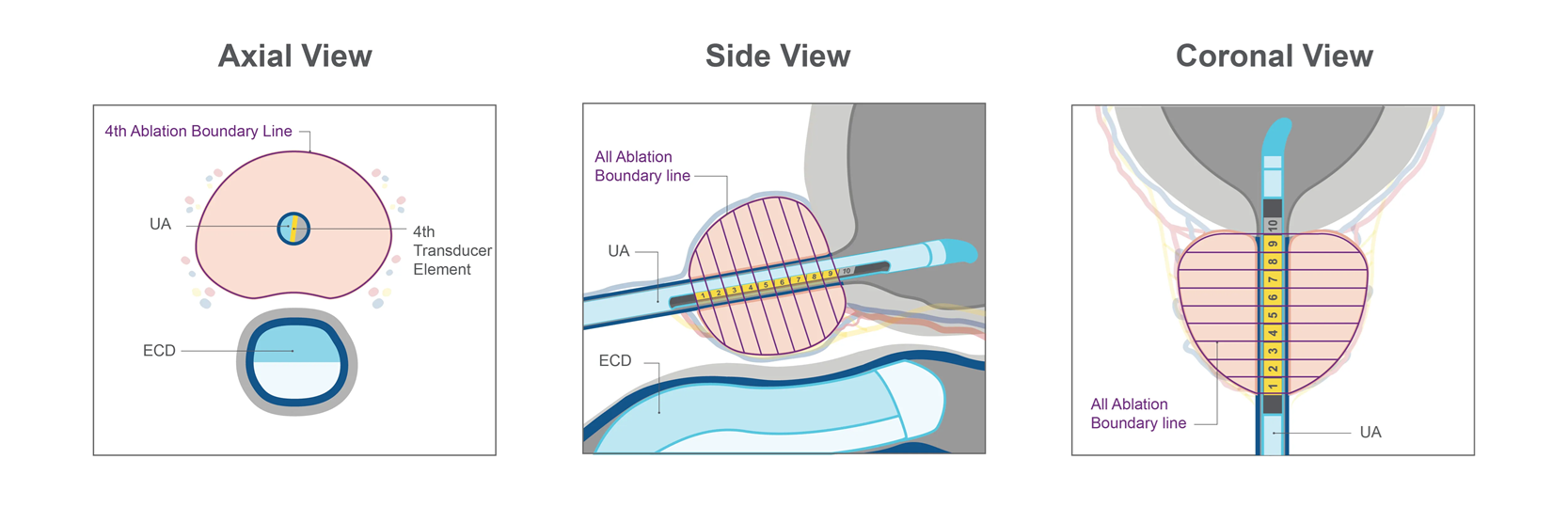
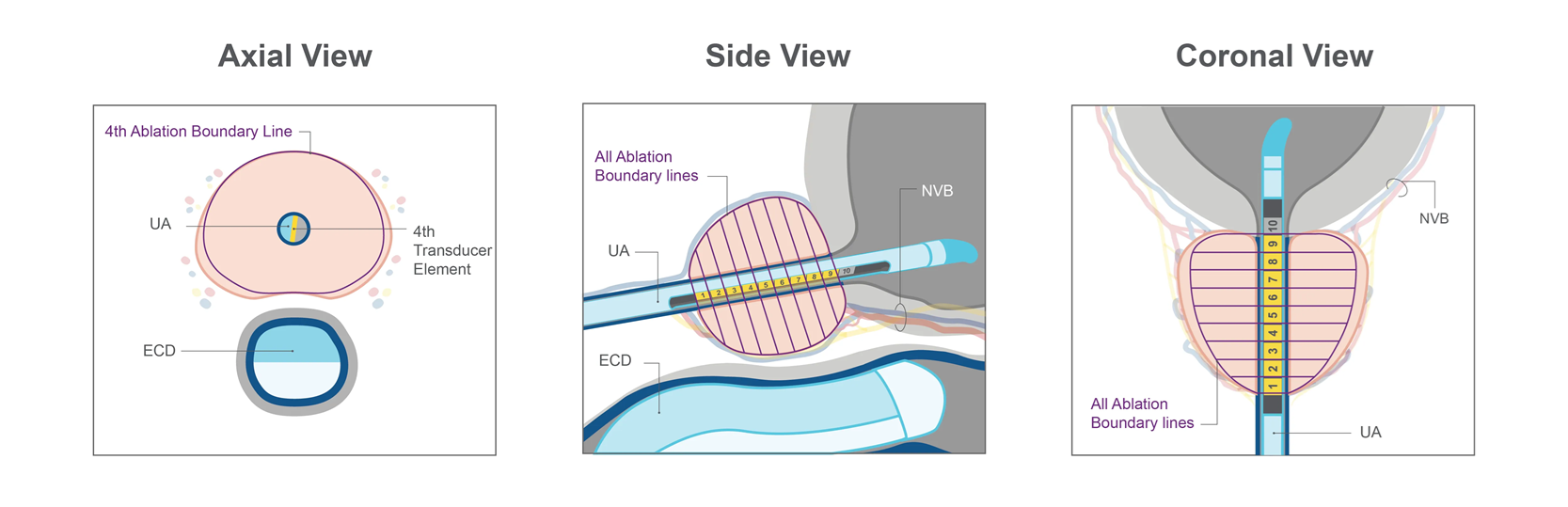
The UA is built with 10 tiny transducer elements. Each one can send ultrasound energy into the prostate, and the doctor can turn them on and off to match the prostate’s size and shape. While they send energy into the prostate, the UA also keeps the urethra cool to shield it from the heat. In the picture below, you’ll see that only 9 out of the 10 elements were enough to reach the target tissue.
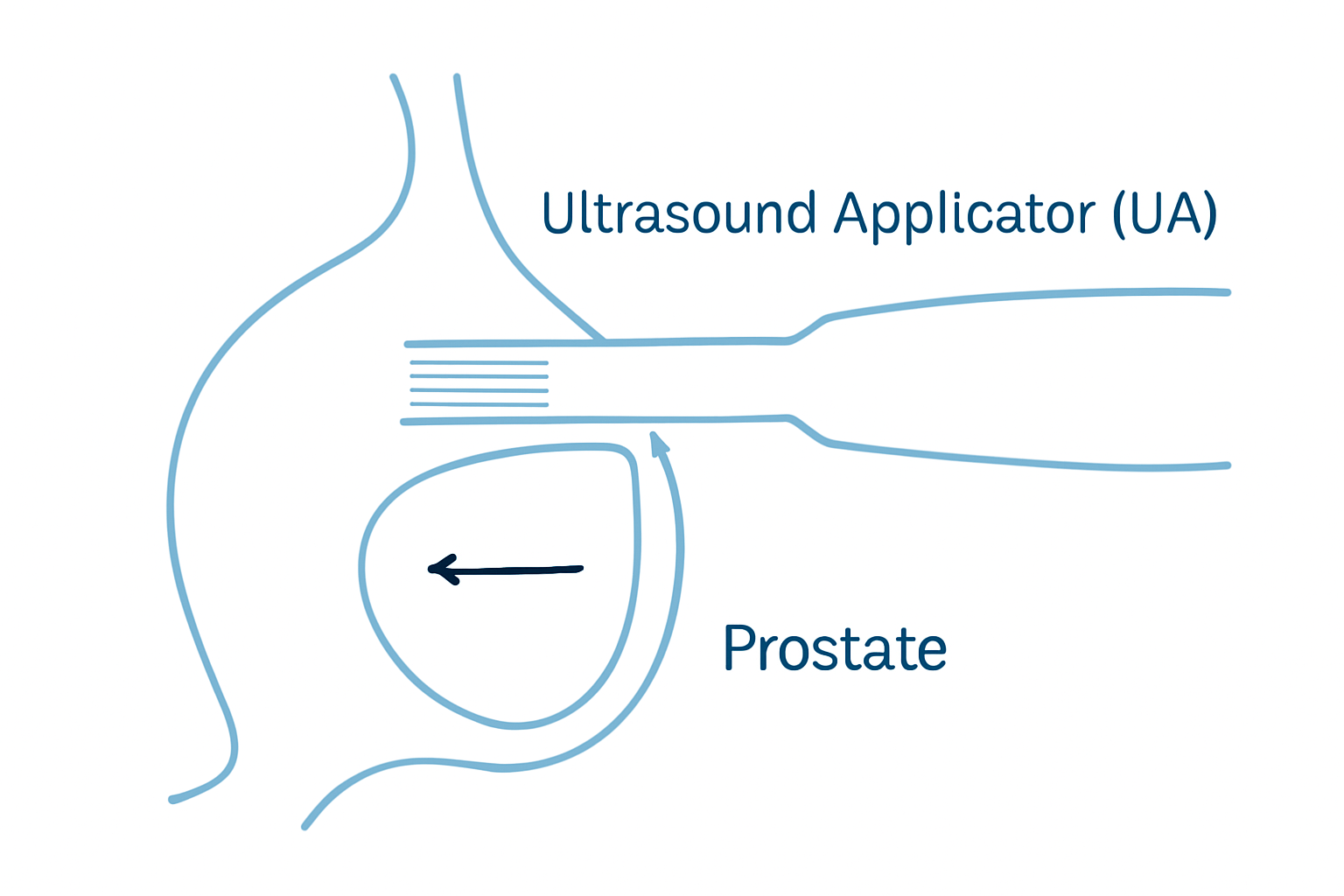
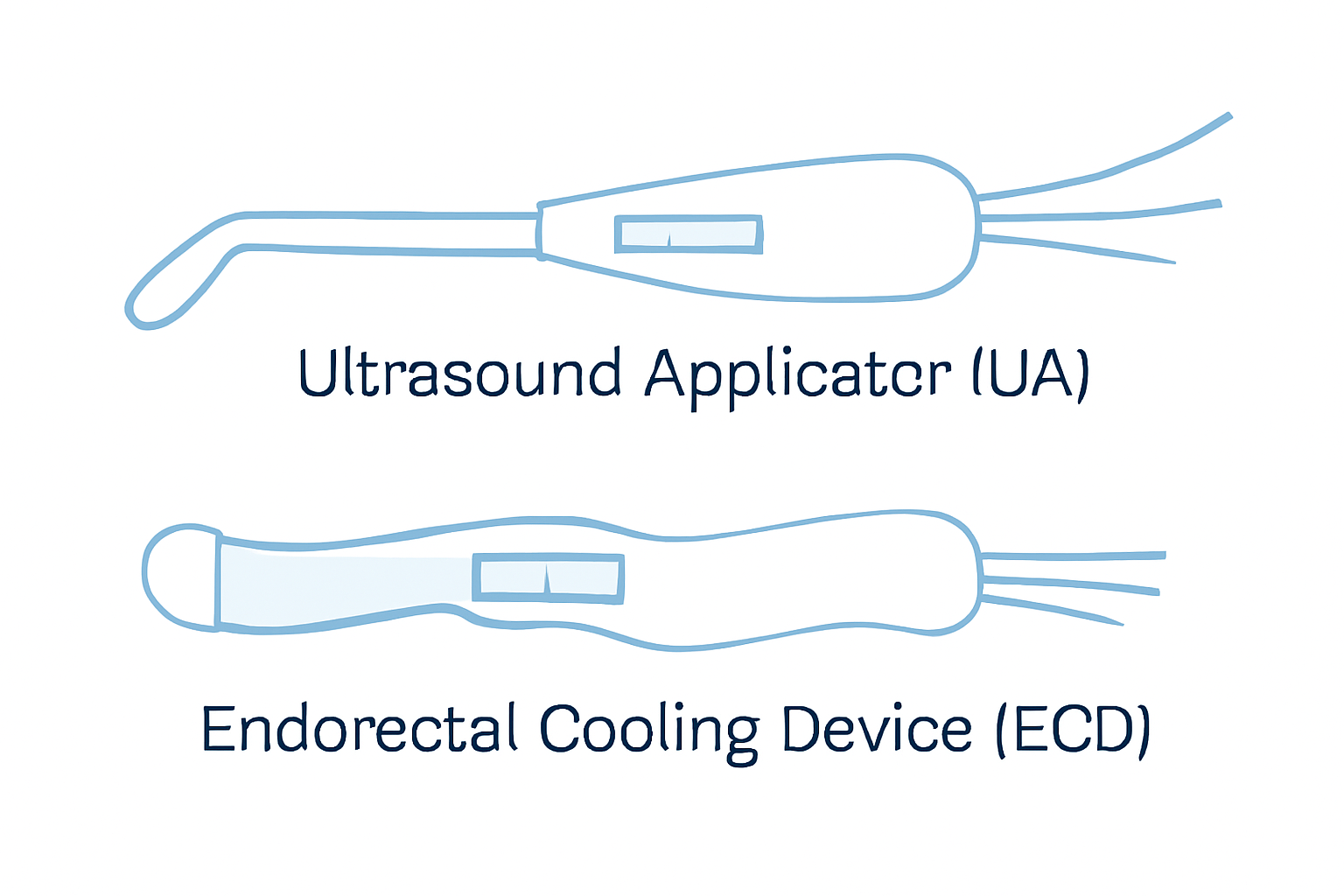
The ECD sits quietly in the rectum and keeps the rectal tissue cool, protecting it from the heat of the ultrasound and helping to preserve the patient’s expected normal functions. It doesn’t make any noise or send out energy.
Once both devices are in place and everything checks out, the treatment team moves on to the planning stage.
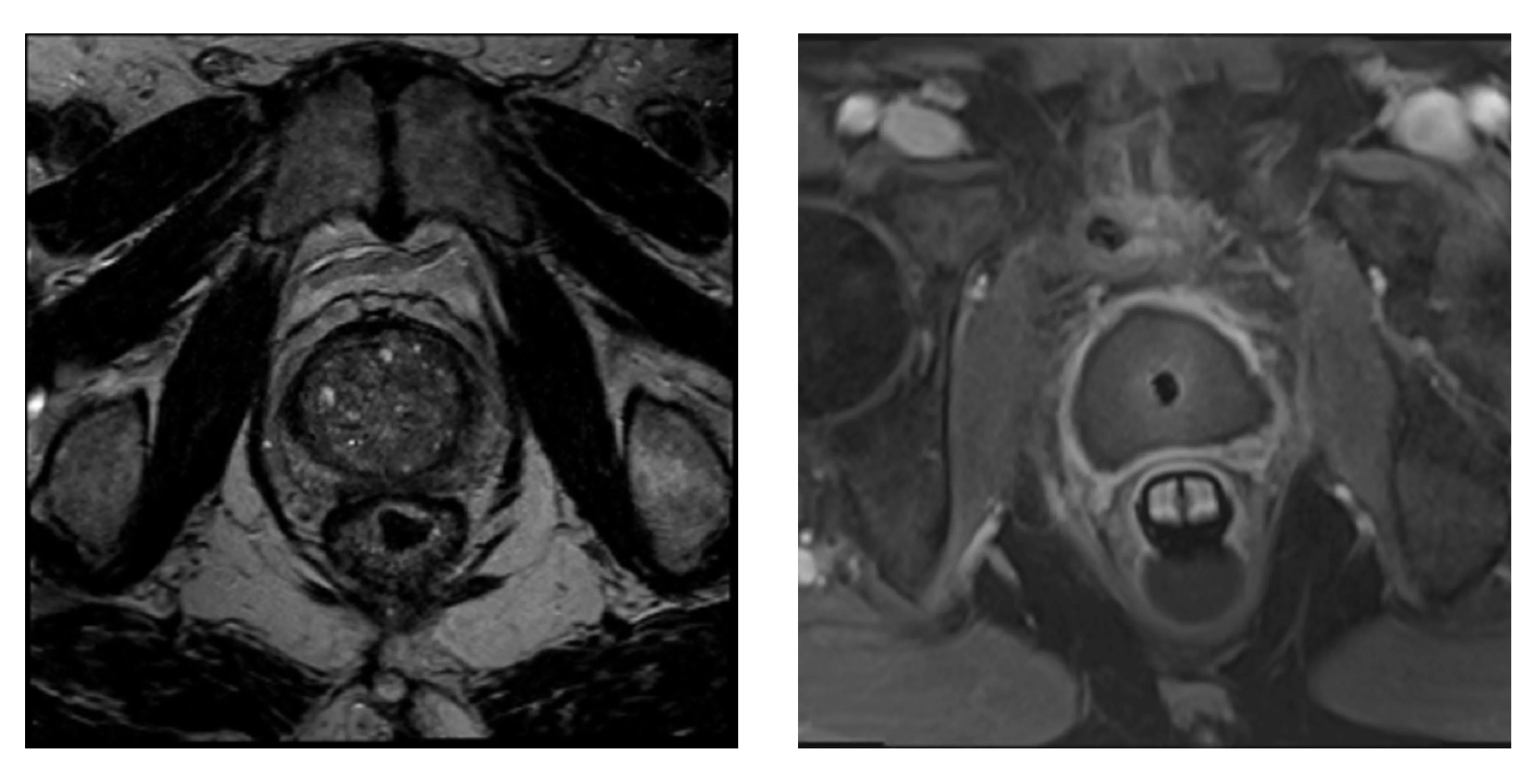
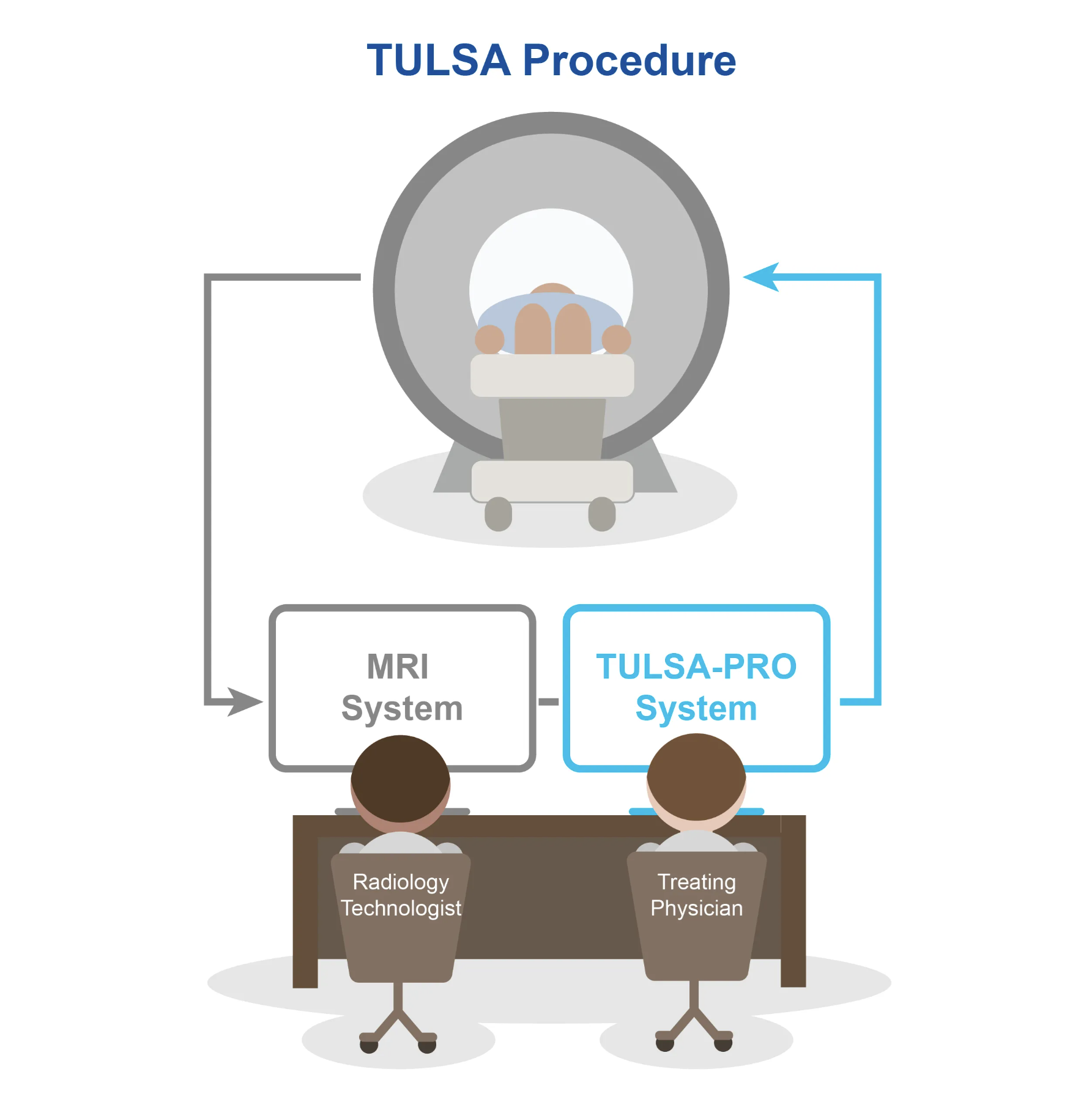
The TULSA-PRO system links directly to the MRI machine. This connection lets the doctor use very detailed MR scans to pinpoint the parts of the prostate that need to be treated.
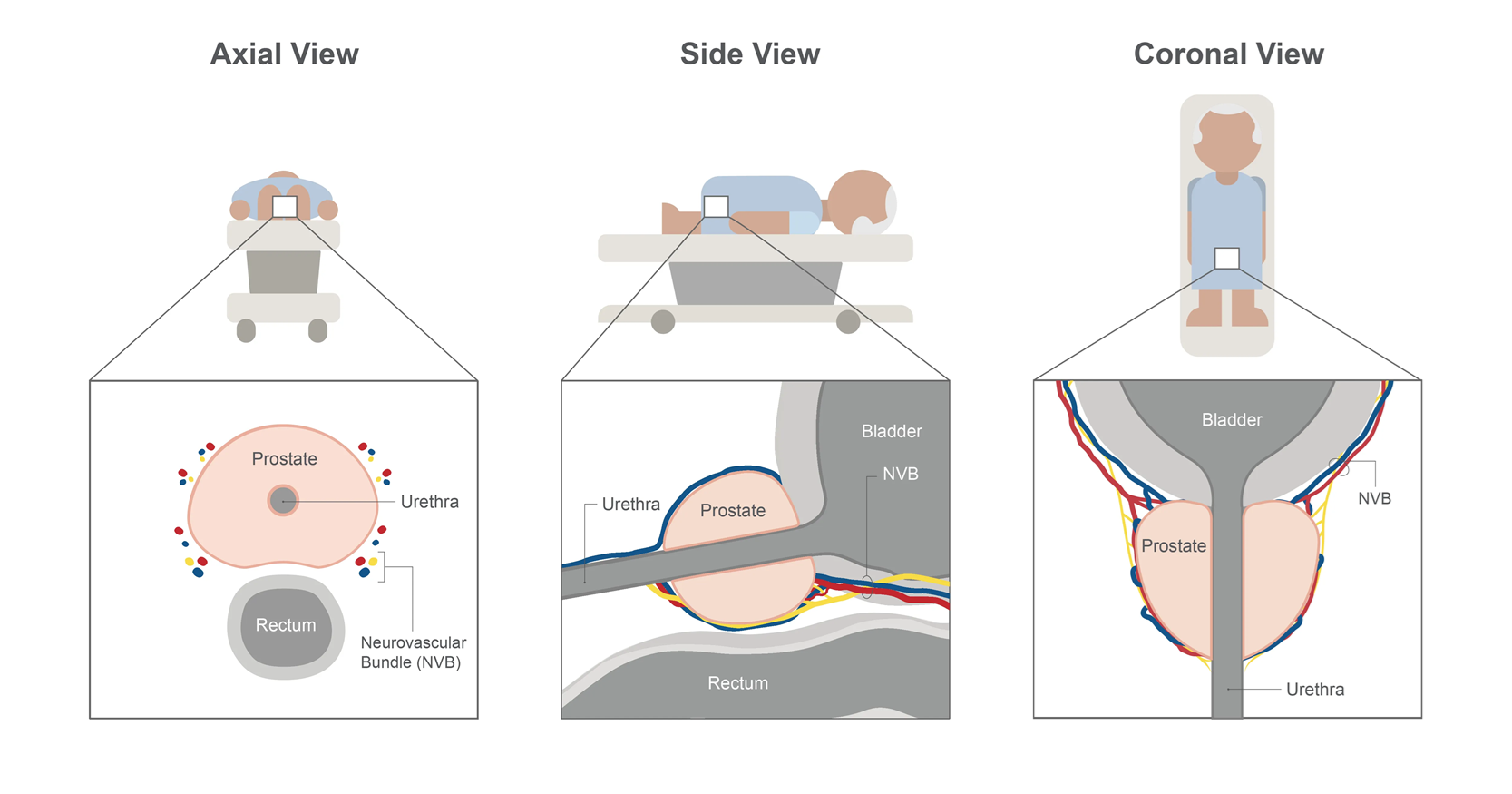
From the MR images, the doctor sketches the outer limits of the area to be treated, creating a unique treatment blueprint that fits the size, shape, and disease of each patient’s prostate, while carefully steering clear of important nerve bundles and other critical structures nearby.
The doctor views the prostate from three angles: axial, sagittal, and coronal. With these three perspectives, the doctor outlines the treatment borders that correspond to each ultrasound element.
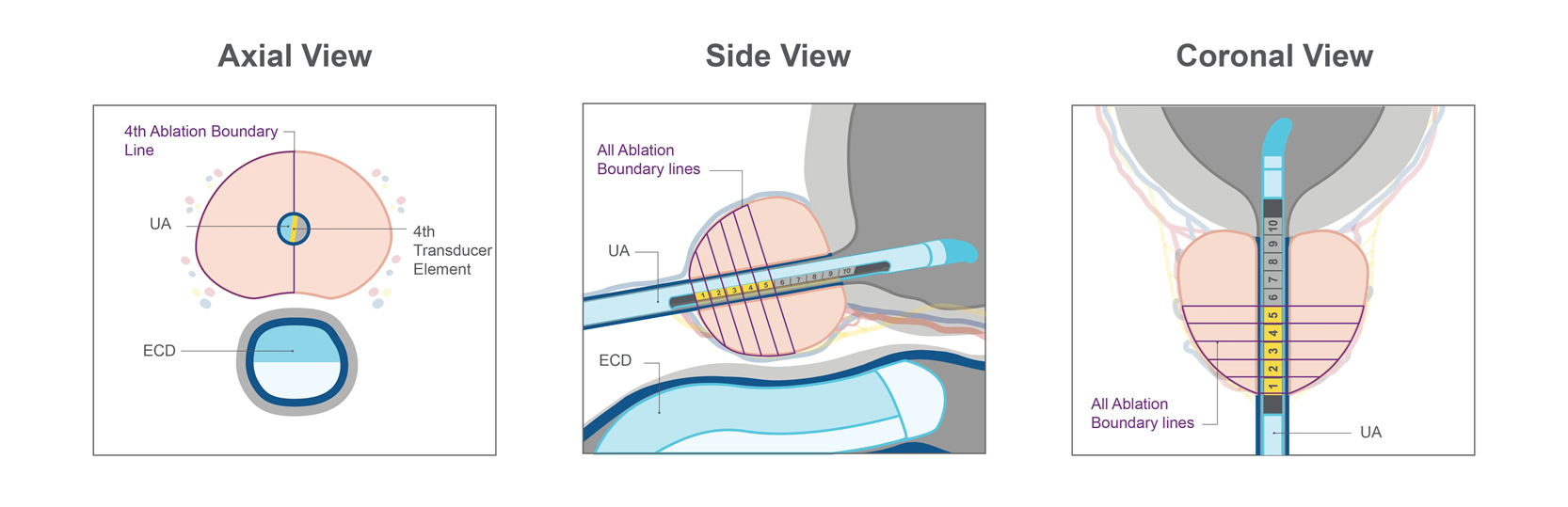
When planning a whole-gland ablation, the doctor continues to add boundary lines for all the remaining ultrasound elements, covering the entire volume of prostate tissue to be treated. If a patient is to undergo a partial-gland ablation, like a hemi-ablation, the doctor can still personalize the treatment by marking only the specific part of the prostate that needs to be treated, and drawing boundaries for only the ultrasound elements that will be active in that section.
Some patients can benefit from a nerve-sparing plan, and doctors can tailor the TULSA Procedure to meet this goal. By moving the ablation boundary lines farther from the neurovascular bundles, the physician creates a safer zone around the nerves. The physician maintains the ability to customize each boundary line according to the patient’s unique anatomy—considering the size and shape of the prostate—as well as the location of unhealthy tissue and the patient’s individual requirements. With the boundary lines now established, the treatment team is prepared to start the prostate ablation.
During ablation, the Ultrasound Applicator rotates within the urethra, producing a gentle, sweeping heating pattern that directs warmth outward and destroys the prostate tissue from the inside out.
The TULSA-PRO system automatically follows the physician’s ablation plan, heating only the tissue inside the boundary lines while providing thermal images in real time. By executing the treatment plan this way, the TULSA-PRO system helps achieve accurate ablation while reducing the chance of human error.
The TULSA-PRO device links directly to the MRI and forms a smart feedback system where temperature maps of the prostate appear on the screen every six seconds. These MRI thermometry images reveal how the temperature of the prostate and surrounding tissue changes in real time, so the doctor can watch the heating process and adjust it if needed. This feedback keeps the TULSA Procedure steady and easy to predict.
After the main ablation step, if the doctor sees that a little more treatment is needed, they can go back and carefully deliver extra energy to that spot on the prostate.
After the last beam, the doctor checks the images again to be sure that the treatment covered the correct prostate zones. Once everything is confirmed, a short catheter is placed, and the patient rests for just a little while in recovery. Most patients can go home the same day, and they usually feel good enough to pick up their regular activities.